Top Reasons for Claim Denials and How to Manage It
Claim denials are one of the most common ways through which health facilities lose income. The loss of income hinders the provision of adequate services to patients. It is, therefore, crucial that the health facility understands what causes the denials in the first place. It is only after establishing the causes that the facility can move to prevent them.
The top claims denial causes include:
Incorrect Patient Information
Before the insurance company releases funds, they have to establish that the patient is the rightful owner of the cover. They rely on medical records to ascertain the users. The validation becomes hard when the information does not tally. Ensure you key in the right patient’s name, date of birth, subscriber number, group, and any other details.
Non-Included Services
While most health insurance covers prevalent diseases, they also provide for limitations. The excluded medications require the patient to cover the whole expenses from out of pocket. Most hospitals are in constant communication with insurance companies for information on included diseases. The insurance companies also tend to update the health facilities in case of any changes. To avoid issues with non-included services, inform the patient they will cover all the expenses before you start offering medication.
Terminated Cover
You can only bill an insurance company for active coverage. Take note of the patient’s cover duration before you include the medical cover. Cases of a defaulting patient can also lead to termination of cover. Liaise with the insurance company to determine the status of the patient’s coverage.
Cost Control
Like any other entity, insurance companies are also after making returns. To achieve this, they tend to reduce expenses by discouraging patients from going for expensive options. The insurance companies are ready to pay for the lower-priced services as you move up, instead of starting with the highest range in the first instance.
Failure to Follow Health Plan Rules
Different health covers come with regulations you have to follow. A breach in any of the provisions allows for the insurance company to deny the claim. If you have doubts about anything, contact the insurance company.
What to Do in Case of Claim Denial
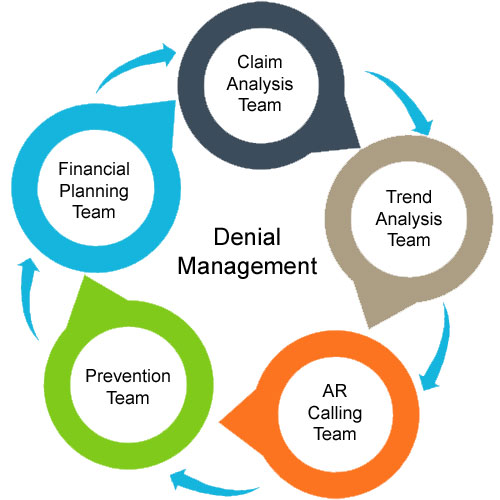
The first step towards better denial management in healthcare is by avoiding the denial in the first place. To help prevent the case, most health facilities are integrating technology into operations. The technology allows for correct data entry as well as availing data on the cover provisions, exemptions, and authorization. The lesser the errors, the lower the chances of denials.
Even with the control measures in place, denial might still happen. This calls for an appeal for the insurance company to overturn the denial. To help medical facilities launch successful appeals, several denial management companies are coming up. These companies come with expertise and experience in creating appeal plans. The team of healthcare advocates understand all the provisions and will help you collect and present your evidence.
Conclusion
Claim denials are detrimental to your health practice. Put in place the right technology to avoid errors leading to the denials. Do not hesitate to contact a reliable denial management solutions provider for a proper denial appeal.
